Diagnostic value of combined magnetic resonance imaging examination of brachial plexus and electrophysiological studies in multifocal motor neuropathy
Abstract
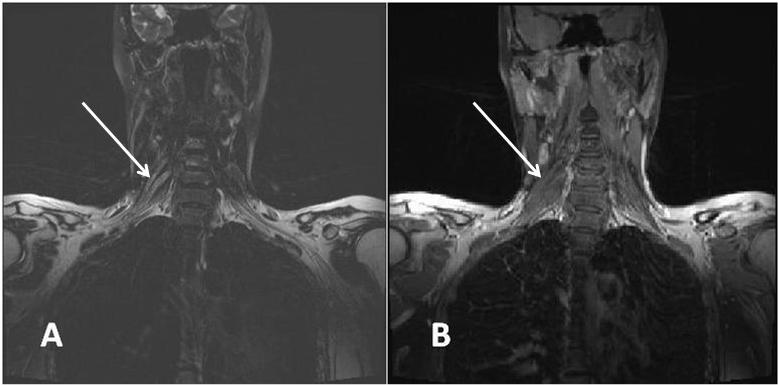
Background/Aim. Multifocal motor neuropathy (MMN) is an immune-mediated disorder characterised by slowly progressive asymetrical weakness of limbs without sensory loss. The objective of this study was to investigate the involvement of brachial plexus using combined cervical magnetic stimulation and magnetic resonance imaging (MRI) of plexus brachialis in patients with MMN. We payed special attention to the nerve roots forming nerves inervating weak muscles, but without detectable conduction block (CB) using conventional nerve conduction studies. Methods. Nine patients with proven MMN were included in the study. In all of them MRI of the cervical spine and brachial plexus was performed using a Siemens Avanto 1.5 T unit, applying T1 and turbo spin-echo T1 sequence, axial turbo spin-echo T2 sequence and a coronal fat-saturated turbo spin-echo T2 sequence. Results. In all the patients severe asymmetric distal weakness of muscles inervated by radial, ulnar, median and peroneal nerves was observed and the most striking presentation was bilateral wrist and finger drop. Three of them had additional proximal weakness of muscles inervated by axillar and femoral nerves. The majority of the patients had slightly increased cerebrospinal fluid (CSF) protein content. Six of the patients had positive serum polyclonal IgM anti-GM1 antibodies. Electromyoneurography (EMG) showed neurogenic changes, the most severe in distal muscles inervated by radial nerves. All the patients had persistent partial CBs outside the usual sites of nerve compression in radial, ulnar, median and peroneal nerves. In three of the patients cervical magnetic stimulation suggested proximal CBs between cervical root emergence and Erb’s point (prolonged motor root conduction time). In all the patients T2-weighted MRI revealed increased signal intensity in at least one cervical root, truncus or fasciculus of brachial plexus. Conclusion. We found clinical correlation between muscle weakness, prolonged motor root conduction time and MRI abnormalities of the brachial plexus, which was of the greatest importance in the nerves without CB inervating weak muscles.
References
Parry GJ, Sumner AJ. Multifocal motor neuropathy. Neurol Clin 1992; 10(3): 671−84.
Nobile-Orazio E, Cappellari A, Priori A. Multifocal motor neuro-pathy: Current concepts and controversies. Muscle Nerve 2005; 31(6): 663−80.
Slee M, Selvan A, Donaghy M. Multifocal motor neuropathy: the diagnostic spectrum and response to treatment. Neurology 2007; 69(17): 1680−7.
Olney RK. Consensus criteria for the diagnosis of partial con-duction block. Muscle Nerve 1999; 22(8): 225−9.
Arunachalam R, Osei-Lah A, Mills KR. Transcutaneous cervical root stimulation in the diagnosis of multifocal motor neuropa-thy with conduction block. J Neurol Neurosurg Psychiatr 2003; 74(9): 1329−31.
van Es HW, Van BLH, Franssen H, Witkamp TD, Ramos LM, Notermans NC, Wokke JH. Magnetic resonance imaging of the brachial plexus in patients with multifocal motor neuropathy. Neurology 1997; 48(5): 1218−24.
Cats EA, Jacobs BC, Yuki N, Tio-Gillen AP, Piepers S, Franssen H, et al. Multifocal motor neuropathy: association of anti-GM1 IgM antibodies with clinical features. Neurology 2010; 75(22): 1961−7.
van Schaik IN, Bouche P, Illa I, Léger JM, van den Bergh P, Cornblath DR, et al. European Federation of Neurological So-cieties/Peripheral Nerve Society guideline on management of multifocal motor neuropathy. Eur J Neurol 2006; 13(8): 802−8.
Meuth SG, Kleinschnitz C. Multifocal motor neuropathy: update on clinical characteristics, pathophysiological concepts and therapeutic options. Eur Neurol 2010; 63(4): 193−204.
Joint Task Force of the EFNS and the PNS. European Feder-ation of Neurological Societies/Peripheral Nerve Society Guideline on management of multifocal motor neuropathy. Report of a Joint Task Force of the European Federation of Neurological Societies and the Peripheral Nerve Society - first . J Peripher Nerv Syst 2010; 15(4) 295−301.
Inaba A, Yokota T, Otagiri A, Nishimura T, Saito Y, Ichikawa T, et al. Electrophysiological evaluation of conduction in the most proximal motor root segment. Muscle Nerve 2002; 25(4): 608−11.
Taylor BV, Gross L, Windebank AJ. The sensitivity and specificity of anti-GM1 antibody testing. Neurology 1996; 47(4): 951−5.
Poceva-Panovska A, Brezovska K, Grozdanova A, Apostolski S, ŠuturkovaLj. Optimization of ELISA method for determina-tion of serum anti-GM1 antibodies. Maced Pharm Bull 2011; 57: 318−20.
Perić S, Lavrnić S, Basta I, Damjanović D, Stosić-Opinćal T, Lavrnić D. Significance of magnetic resonance imaging in differential diagnosis of nontraumatic brachial plexopathy. Vojnosanit Pregl 2011; 68(4): 327−31.
Van Asseldonk JH, Franssen H, Van Berg-Vos RM, Wokke JH, Van Berg LH. Multifocal motor neuropathy. Lancet Neurol 2005; 4(5): 309−19.
Bouche P, Moulonguet A, Younes-Chennoufi AB, Adams D, Baumann N, Meininger V, et al. Multifocal motor neuropathy with con-duction block: a study of 24 patients. J Neurol Neurosurg Psy-chiatr 1995; 59(1): 38−44.
Nguyen TP, Chaudhry V. Multifocal motor neuropathy. Neurol India 2011; 59(5): 700−6.
Katz JS, Saperstein DS. Asymmetric Acquired Demyelinating Polyneuropathies: MMN and MADSAM. Curr Treat Options Neurol 2001; 3(2): 119−25.
Azulay JP, Blin O, Pouget J, Boucraut J, Billé-Turc F, Carles G, et al. Intravenous immunoglobulin treatment in patients with motor neuron syndromes associated with anti-GM1 antibodies: a double-blind, placebo-controlled study. Neurology 1994; 44(3 Pt 1): 429−32.
O'Ferrall EK, White CM, Zochodne DW. Demyelinating symme-tric motor polyneuropathy with high titers of anti-GM1 anti-bodies. Muscle Nerve 2010; 42(4): 604−8.
Kuwabara S, Cappelen-Smith C, Lin CS, Mogyoros I, Bostock H, Burke D. Excitability properties of median and peroneal motor axons. Muscle Nerve 2000; 23(9): 1365−73.
Burke D, Kiernan MC, Bostock H. Excitability of human axons. Clinical neurophysiology 2001; 112(9): 1575−85.
Van Berg-Vos RM, Franssen H, Wokke JH, Van Es HW, Van Berg LH. Multifocal motor neuropathy: diagnostic criteria that predict the response to immunoglobulin treatment. Ann Neu-rol 2000; 48(6): 919−26.
Katz JS, Barohn RJ, Kojan S, Wolfe GI, Nations SP, Saperstein DS, et al. Axonal multifocal motor neuropathy without conduction block or other features of demyelination. Neurology 2002; 58(4): 615−20.
Van Es HW. MRI of the brachial plexus. Eur Radiol 2001; 11(2): 325−36.
Wittenberg K, Adkins MC. MR imaging of nontraumatic brachial plexopathies: frequency and spectrum of findings. Radiographics 2000; 20(4): 1023−32.